University of Guelph researchers have developed a hand-held thermal camera-based imaging tool that may improve COVID-19 screening protocols.
Used at screening locations, the device could quickly detect higher heart rate, body temperature or breathing rate – all potential indicators of COVID-19 infection. Users can flag individuals for further testing, preventing them from unknowingly spreading the virus, and improve triage and monitoring in hospitals, said Dr. Andrew Hamilton-Wright, a professor in the School of Computer Science.
“We’re hoping to play a part in lowering the spread of the virus with our new innovation,” said Hamilton-Wright. “Having better tools to improve public health outcomes is a big win for everybody.”
Hamilton-Wright and M.Sc. student Kassy Raymond led a team of U of G co-op students including Tessa Brenders and Brayden Klemens and Alex Dunn from Ryerson University. They worked with IRIS Research and Development Group, based in Burlington, Ont., and St. Joseph’s Healthcare Hamilton.
Hamilton-Wright and Raymond combined their computer science expertise to assess three key health measures – heart rate, breathing rate and skin temperature – to be deployed using a thermal camera being developed by IRIS Research and Development Group.
The camera-based measurement requires no direct physical contact and can operate at a distance from potentially infectious patients. The tool can also be controlled remotely.

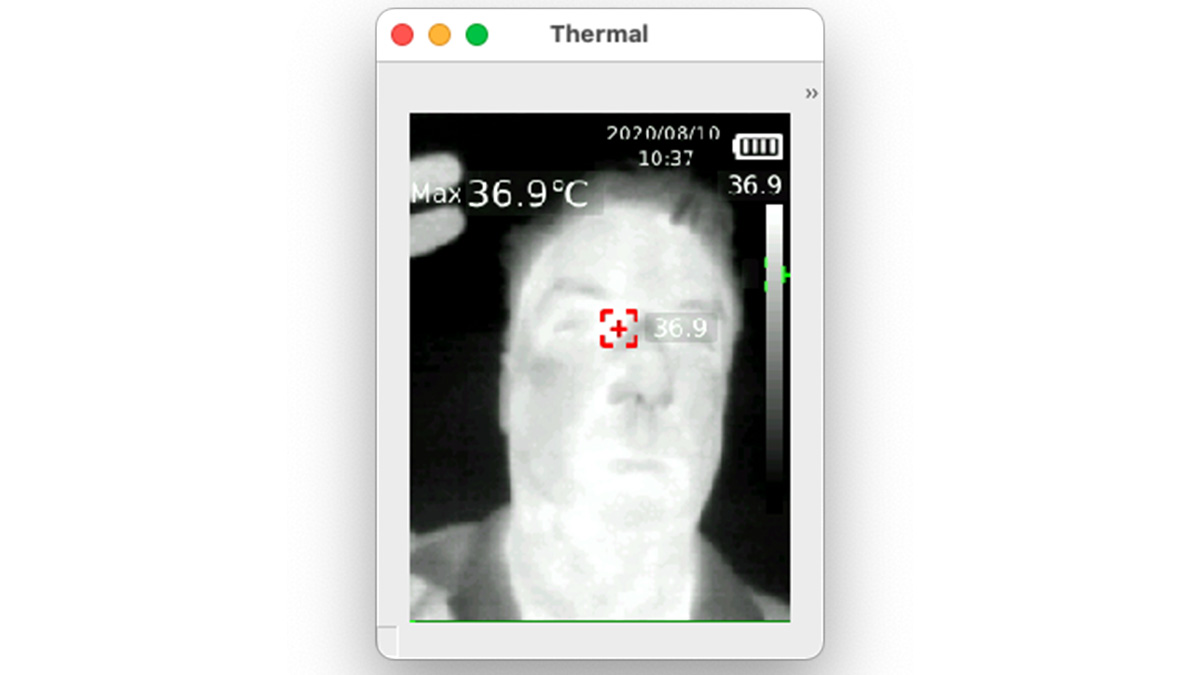
Their device takes 15 thermal images per second of a person’s face. Then, using machine learning and the Python programming language, the tool can identify regions of the face such as the nose and mouth.
A colour change is expected in the thermal images if the temperature is higher than normal in these areas. The device can also measure breathing rate and heart rate using computer algorithms developed by the team.
The researchers worked to account for factors that could affect the camera’s accuracy, including varying thermal readings based on a person’s race, for example, or someone wearing makeup.
They are currently collecting data to assess the effectiveness of their device. The research team has partnered with St. Joseph’s Health Network in Ontario to test the tool on intensive care unit patients.
St. Joseph’s Health Network has expressed interest in using the device to improve patient outcomes. The team also plans to commercialize the tool and make it available for different organizations.
“We’re passionate about promoting the benefits of machine learning to drive positive health outcomes,” says Raymond. “If our tool can potentially reduce the spread of the virus, we know that we’re making an extremely positive impact.”
This research is supported by the University of Guelph COVID-19 Research Development and Catalyst Fund.
Contact:
Dr. Andrew Hamilton-Wright
andrew.hamilton-wright@uoguelph.ca